The growing popularity of GLP-1 receptor agonists—including Ozempic and Wegovy from Novo Nordisk, and Mounjaro and Zepbound from Eli Lilly—has added fuel to an already fiery debate over the government’s role in subsidizing access to these drugs. Originally developed for Type 2 diabetes, these medications have proven highly effective for treating obesity—a chronic condition affecting more than 40% of U.S. adults. However, with costs often exceeding $1,000 per month for patients who are under- or uninsured, these treatments remain out of reach for many Americans.
Medicare currently limits its coverage of GLP-1s to individuals with Type 2 diabetes or certain heart conditions, excluding prescriptions aimed solely at obesity. Medicaid coverage of GLP-1s for obesity, however, varies by state. While all state Medicaid programs include GLP-1s prescribed for Type 2 diabetes, only 36 states cover at least one of the FDA-approved GLP-1s for obesity (Wegovy, Zepbound, or Saxenda).
Amid the Biden administration’s recent proposal to expand obesity drug coverage under Medicare and Medicaid, experts at Real Chemistry examined which state Medicaid programs currently cover GLP-1s approved to treat obesity and how much they are spending. This study uses Real Chemistry’s IRIS market intelligence platform, which includes over ten years of medical, hospital, and pharmacy claims data from more than 300 million U.S. patients. It examines how state Medicaid coverage for GLP-1 medications varies and the financial impact of these coverage differences.
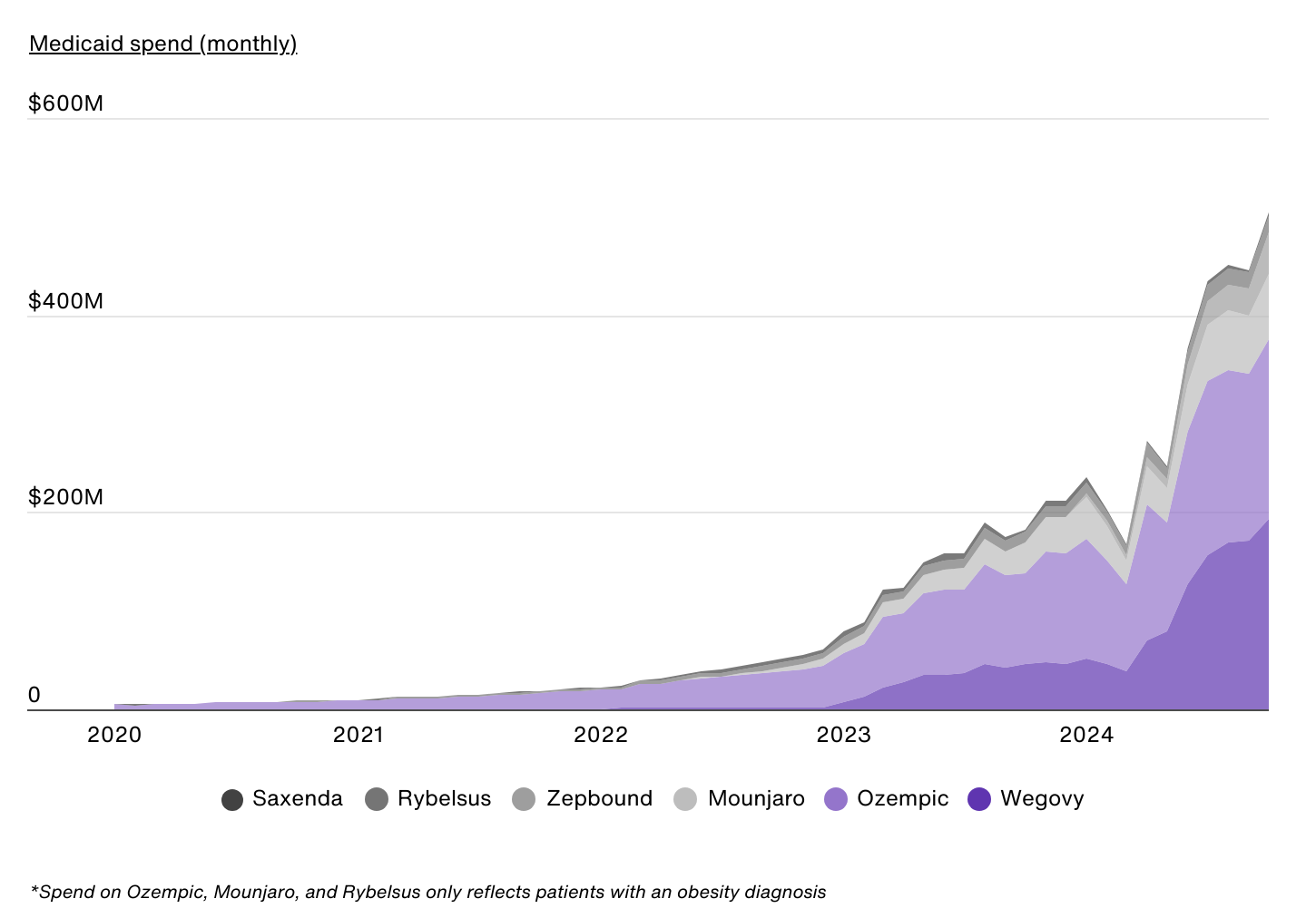
How Much Does Medicaid Currently Spend on GLP-1s for Obesity?
Data Source: IRIS by Real Chemistry | Image Credit: Real Chemistry
Medicaid spending on GLP-1s has grown exponentially over the past five years, reflecting both an increase in GLP-1 usage and expanded coverage in many states. This figure includes expenditures on both obesity-indicated GLP-1s and Type 2 diabetes-indicated GLP-1s prescribed to patients with an obesity diagnosis. In January 2020, spending on Ozempic, a Type 2 diabetes-indicated GLP-1, was just $4.6 million, while Wegovy—one of the most prominent FDA-approved GLP-1s for weight management—had not yet been introduced. By January 2024, monthly Medicaid spending on Wegovy alone exceeded $51 million, and by October 2024, it had grown to $192 million.
This rapid spending increase is the result of two primary factors. First, more Medicaid enrollees are being prescribed GLP-1s for obesity. Second, several states expanded Medicaid coverage to include GLP-1s specifically approved for obesity, such as Wegovy and Zepbound. This combination of increased usage and expanded state coverage has increased Medicaid spending on GLP-1s for obesity to more than $500 million in October 2024 alone, with total expenditures reaching $3.5 billion over the past 12 months.
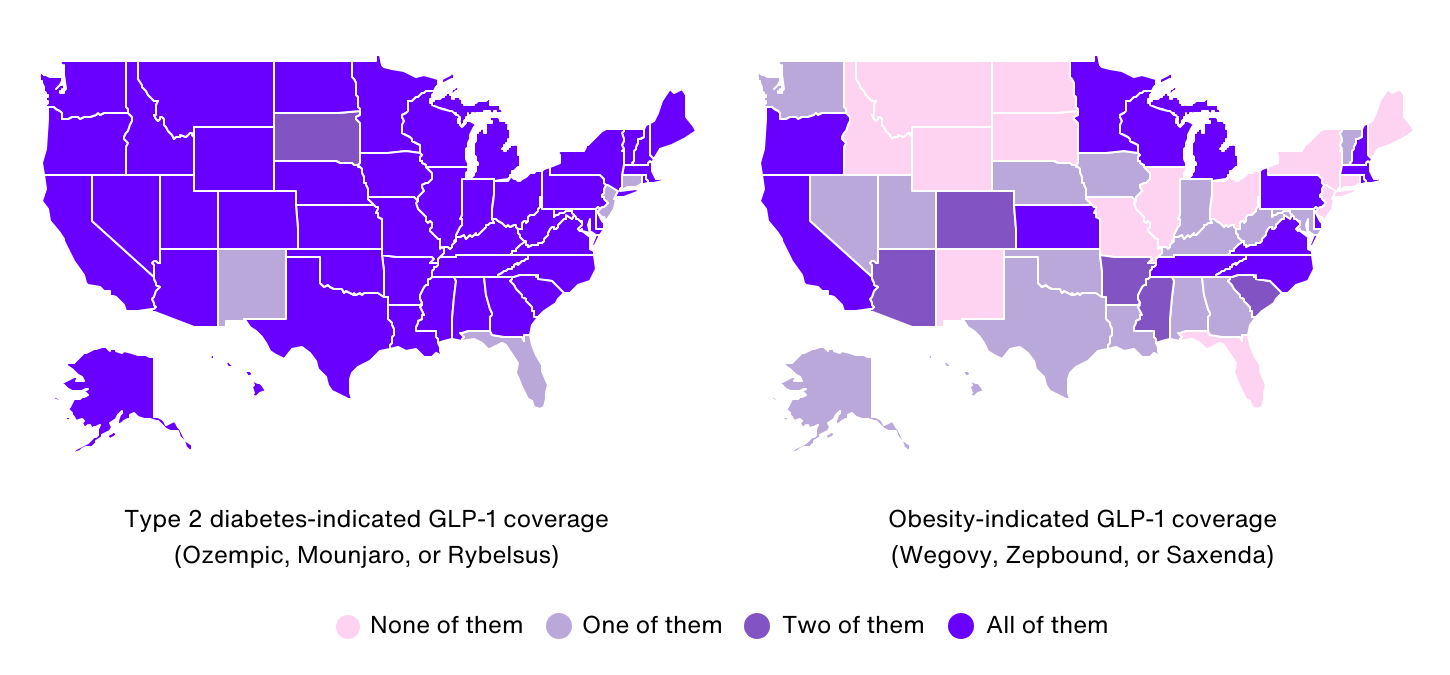
Which State Medicaid Programs Currently Cover GLP-1 Drugs?
Data Source: IRIS by Real Chemistry | Image Credit: Real Chemistry
Medicaid coverage for GLP-1s, both for Type 2 diabetes and obesity, varies widely across the United States. While all states cover at least one Type 2 diabetes-indicated GLP-1, coverage for obesity-indicated options is less consistent.
States Offering Broad GLP-1 Coverage for Obesity
A total of 14 states, including California, Michigan, and Pennsylvania, provide Medicaid coverage for the most common GLP-1s approved for both Type 2 diabetes and obesity. In these states, beneficiaries have access to Wegovy, Zepbound, and Saxenda, alongside Type 2 diabetes-indicated options such as Ozempic, Mounjaro, and Rybelsus.
States Offering Partial GLP-1 Coverage for Obesity
Another 22 states, including Texas, Arizona, and Washington, offer partial coverage for obesity-specific GLP-1s. These states typically include Wegovy and sometimes Saxenda or Zepbound in their Medicaid coverage lists.
States With No Coverage for Obesity-Indicated GLP-1s
In 14 states and the District of Columbia, Medicaid programs do not cover GLP-1s for obesity. Beneficiaries in these states, which include residents of New York, Illinois, and Ohio, can only access GLP-1s like Ozempic, Mounjaro, or Rybelsus if they have a Type 2 diabetes diagnosis. They currently don’t have access to Wegovy, Zepbound, or Saxenda under their Medicaid benefits.
States With Limited Type 2 Diabetes GLP-1 Coverage
A smaller subset of the states mentioned above with no coverage for obesity-indicated GLP-1s—including the District of Columbia, Florida, and New Jersey—also limits coverage for Type 2 diabetes-indicated GLP-1s. In these states, Medicaid coverage for Rybelsus or Mounjaro may be excluded, even though Ozempic is approved on the state’s Medicaid formulary.
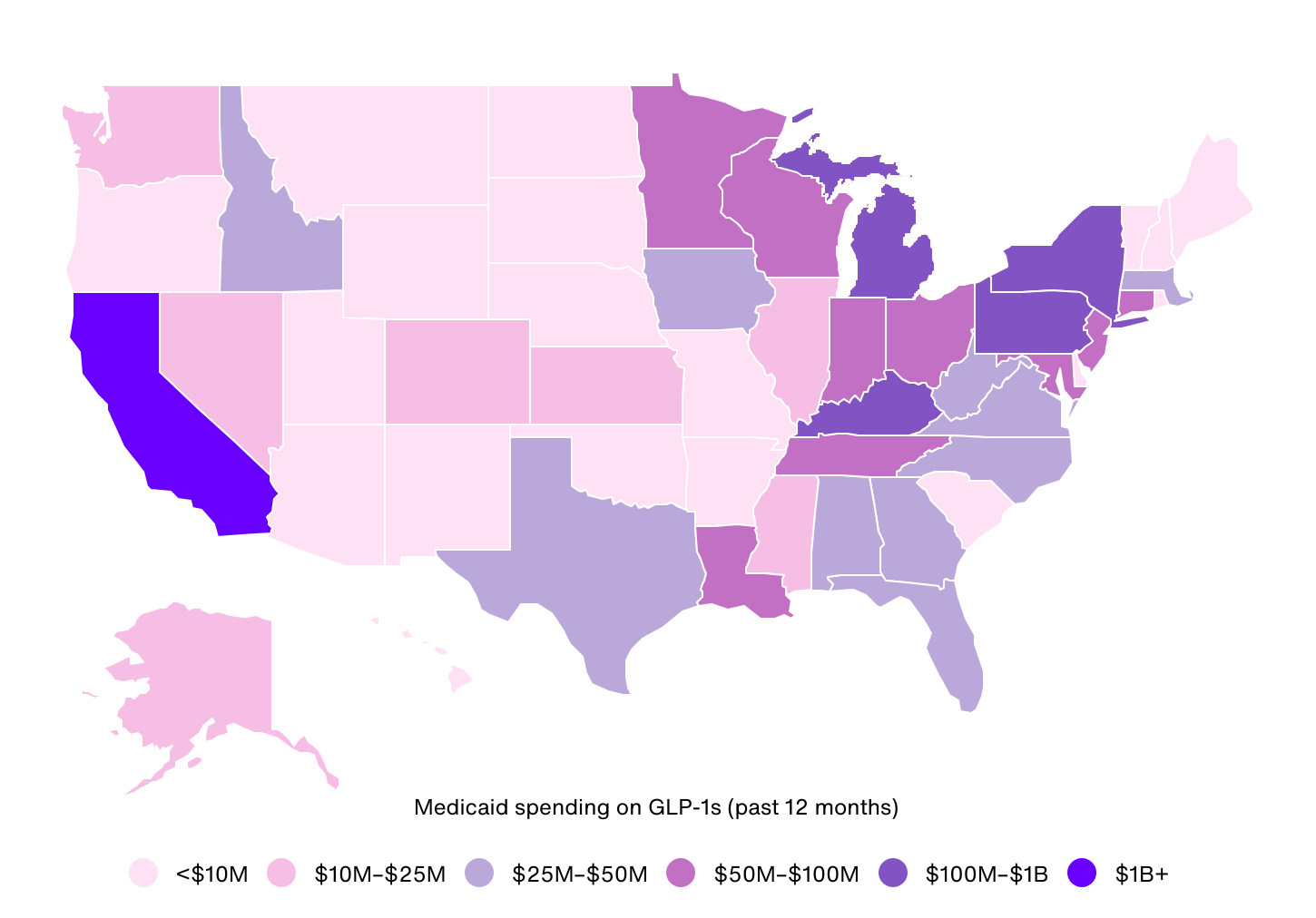
Medicaid Spending on GLP-1 Drugs by State
Data Source: IRIS by Real Chemistry | Image Credit: Real Chemistry
Nationally, Medicaid spending on GLP-1s totaled $3.5 billion between November 2023 and October 2024, averaging $48 per Medicaid enrollee. However, spending varies widely by state, reflecting differences in coverage policies and population needs.
California’s Medicaid program led the nation in total spending, exceeding $1.4 billion, or $118 per enrollee—the second highest per-capita spending. This total represents a 235% year-over-year increase, driven by the state’s large population and comprehensive coverage of all major obesity- and Type 2 diabetes-indicated GLP-1s. Pennsylvania ranked second overall in total Medicaid spend, with nearly $298 million in total spending and $106 per enrollee. Similar to California, Pennsylvania’s spending grew 232% year over year.
Kentucky stands out for having the greatest spending per enrollee at $162, despite ranking third in total spending. Unlike California and Pennsylvania, which provide broad coverage for all obesity-indicated GLP-1s, Kentucky’s Medicaid program covers only Wegovy for weight management alongside Type 2 diabetes-indicated medications. The states with the lowest spending, North Dakota and Wyoming, don’t provide Medicaid coverage for any of the obesity-indicated GLP-1s.
Methodology

Photo Credit: Nito / Shutterstock
The data used in this study comes from IRIS by Real Chemistry—a proprietary market intelligence platform fueled by billions of data points, including medical, hospital, and pharmacy claims covering more than 300 million U.S. patients over 10 years. Additional statistics on Medicaid enrollment were sourced from the Centers for Medicare & Medicaid Services.
For this analysis, GLP-1 Medicaid spend is the estimated amount of money in U.S. dollars that Medicaid has spent on the most common GLP-1s (Ozempic, Mounjaro, Rybelsus, Saxenda, Wegovy, and Zepbound). Although Ozempic, Mounjaro, and Rybelsus are not FDA-approved for obesity treatment, they are included in the analysis due to the high number of patients with an obesity diagnosis using these products compared to other FDA-approved Type 2 diabetes GLP-1 agonists. That said, spending on Ozempic, Mounjaro, and Rybelsus is only included for patients who have an obesity diagnosis; whereas, spending on Saxenda, Wegovy, and Zepbound is included regardless of obesity diagnostic claims.
States were ranked based on total Medicaid spend on these GLP-1 drugs between 11/1/23 and 10/31/24. Note that spending totals are estimates generated by comparing previous government data figures from Medicaid’s State Drug Utilization Database to real-time claims data. State-level Medicaid coverage indicates whether an individual state includes obesity-indicated GLP-1s (Saxenda, Wegovy, and Zepbound) or Type 2 diabetes-indicated GLP-1s (Ozempic, Mounjaro, and Rybelsus) on its formulary or preferred drug list, including non-preferred or restricted coverage.
For complete results, see Which State Medicaid Programs Cover GLP-1s for Weight Loss & How Much Are They Spending? on Real Chemistry.
